Association of Anaesthetists/Barema Joint Research Grants
The successful applicants for the Association of Anaesthetists/Barema Joint Research Grants were:
Please click the arrows to view each abstract
Dr James Bowness & Dr Helen Higham
University of Oxford
Title
Pilot Study to Evaluate the Scientific Basis and Impact of Assistive Artificial Intelligence Technology for Ultrasound Image Interpretation in Ultrasound-Guided Regional Anaesthesia
Amount
£3,237
Scientific Abstract
Regional anaesthesia can help to improve patient care, but is often delivered by a limited number of experts, restricting patient access. Ultrasound-guidance achieves the most efficacious outcomes, but relies on accurate interpretation of sono-anatomy. Human medical image analysis is proven to be imperfect. Artificial intelligence systems that aid the recognition of salient features on ultrasound could support performance and training, and enhance patient access to these techniques.
This pilot study, endorsed by Regional Anaesthesia UK, will use AnatomyGuide™ (Intelligent
Ultrasound, Cardiff, UK) as an example of such a system.
Accuracy of AnatomyGuide™ identification of anatomical structures on ultrasound will be compared to a panel of experts. Subsequently, anaesthetists (of varying experience/expertise) will be recruited from four centres in the UK. They will evaluate the ultrasound scans, marking anatomical boundaries, with and without the use of AnatomyGuide™
Outcomes assessed:
- Accuracy of recognition of anatomical structures
- Time taken
- Confidence
- Eye tracking characteristics
- Assessments of cognitive load during image analysis
Outcomes will be compared between anaesthetists (without AnatomyGuide™), to identify performance characteristics by level of experience/expertise. Differences associated with the use of AnatomyGuide™ will then be assessed, to gauge the potential of such technology to facilitate enhanced performance.
Dr Brendan A McGrath
Manchester University Hospitals NHS Foundation Trust
Title
Improving voice quality, intelligibility and laryngeal function during above-cuff tracheostomy vocalisation
Amount
£32,842
Scientific Abstract
Tracheostomies are 'artificial airways' used in the Intensive Care Unit (ICU) for patients requiring prolonged ventilatory support, or for patients with altered airway anatomy. Annually c.20,000 new tracheostomies are inserted (UK). Awake patients often cannot vocalise as tubes have a balloon/cuff 'sealing off' the upper airway to mitigate aspiration and/or facilitate ventilation. Pilot research demonstrated early restoration of trans-laryngeal airflow improves laryngeal function, improves coughing, and provides the gift of speech. We aim to 'fine tune' the delivery of airflow to optimise the voice quality and speech produced by above-cuff vocalisation (ACV).
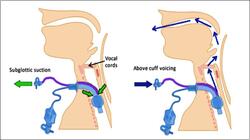
Figure 1. Usual subglottic suction drainage of material that enters the airway and sits above the cuff (left) and the ACV gas flow delivered in the opposite direction so that flow crosses the larynx and exits via the mouth, allowing speech and laryngeal function (right).
Our current NIHR-i4i project produced a prototype ACV device generating crude speech. Voice quality, speech intelligibility and coughing with ACV haven't been previously investigated or reported. We hypothesise that voice quality/intelligibility and laryngeal function (coughing) are influenced by ACV gas flows (flow, timing, warmth and humidification). Primary research question: can we optimise the delivery of ACV to improve resulting voice quality (assessed by CAPE-V tool).
We propose an adjunctive study to record and analyse voice and cough in tracheostomised critically ill patients using established tools, in collaboration with Speech & Language, Respiratory Medicine and the Manchester Centre for Audiology and Deafness, developing innovative techniques to improve care.







