DAS Small Grants
Please click the arrows to view each abstract
To determine the optimal endotracheal tube diameter for cricothyroidotomy and to assess the effect of the tracheal hook on cricothyroid membrane height
Dr Kim Caulfield
Background
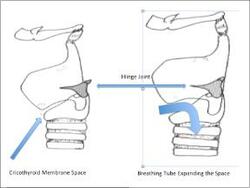
Cricothyroidotomy is an emergency procedure used by doctors and paramedics to provide oxygen to critically unwell patients when it cannot be provided any other way. Creating a hole in the front of the neck and placing a tube through it does this. This tube passes through skin and then through a narrow space called the cricothyroid membrane before entering the normal airway tube (trachea). The tube that is currently recommended for this is 8.2 mm thick on the outside. This thickness is considered important to let oxygen and other gases flow freely inwards and outwards. The membrane was previously thought to be about 10 mm high and would permit passage of the slightly smaller tube. However, recent research done by doctors, including ourselves using existing neck scans suggests that the membrane may be smaller than expected in a significant number of patients and that smaller tubes maybe required. We have reason to believe and wish to investigate whether the membrane space is expandable i.e. can move apart while the tube is passing through it. We believe this is the case because of a hinge type joint at the junction of the two cartilages on either side of the space where they join together at the back of the upper airway tube (Figure1).
Methods
We propose to do a two-phase study. Using commercially purchased animal tracheas we will assess the effect of different incision sizes (length of cut through the membrane) on its expandability. We anticipate that a longer cut will result in more expandability. We will try and pass a sequence of breathing tubes from small to large through each cut starting with small tubes and working up to determine the biggest tube that can fit through each membrane. In the second phase of the study we will hide a trachea under synthetic skin and ask doctors to perform the simulated procedure with the largest tube that can fit though the membrane to see if it fits in a clinical simulation. We also wish to examine if a medical device called a hook makes the membrane bigger and allows bigger tubes to pass.
These doctors will be already trained in these techniques and would be expected to perform this procedure in an emergency. The study will be carried out in a disused operating theater used for training.
Feasibility
We have already performed and published related work in this field both in x-ray measurement and performance of this technique with similar animal specimens.
Value of this information
We hope to contribute to patient safety by assessing performance of currently recommended equipment and techniques.
Figure1
'Obese neck' training manikin project
Dr Christopher Gough
Background
In an emergency, when an asleep patient cannot have a tube passed down into their airway (intubate), and it is not possible to maintain their oxygen levels in another way, the rescue technique is to make a cut in the front of the neck, and to pass a tube through this into the trachea - the main airway to the lungs. This rescue technique is called an emergency front of neck airway (eFONA).
A national project has shown that establishing eFONA is very challenging, and is unsuccessful in the majority of cases where is attempted. Patients reported to the project were twice as likely to be obese, and four times as likely to be morbidly obese, compared to the general population. Patients requiring eFONA are more likely to be obese than slim.
We know that patients who are more difficult to intubate have, on average, an increased distance between the skin at the front of the neck and the entry to trachea. However, the manikins used to practice the eFONA technique mimic patients with a "slim neck" rather than an obese neck.
We have previously shown that when a piece of pork-belly is added to a standard "slim neck" manikin, to simulate an obese neck, then during simulated eFONA the time taken to successfully get a breathing tube into the trachea, and the failure rates, both increased to levels seen in clinical practice.
Although this study showed the value of this obese neck model, fresh pork belly meat is impractical for general use for a number of reasons, including food poisoning, cost and significant preparation time. At present there is no obese neck manikin commercially available.
We wish to evaluate a newly developed manikin which mimics the neck of an obese patient, and compare it to the slim neck manikin and the pork belly manikin used in our previous study. We aim to improve eFONA training and improve patient safety associated with airway management.
Methods
We propose to use senior members of the anaesthetic department at the Royal United Hospital Bath to manage a 'cannot intubate, cannot oxygenate' situation, involving each of three training manikins:
1. a pork belly-modified training manikin to simulate an obese patient
2. an un-modified manikin to simulate a slim patient
3. a newly developed obese neck simulation manikin from a commercial company
Equipment will be provided in accordance with national guidelines for the management of this situation, and participants will be excluded if they have not had recent eFONA training. The order in which the manikins are presented will be randomised to prevent rehearsal bias.
Each participant will be issued a unique anonymised number to allow them to be compared across their three manikin attempts. The investigators will record:
1. Time to first effective ventilation
2. Success within 20 minutes - Y/N
After the eFONA attempts, the participant will be asked to give feedback on each of the manikins.
Comparative study evaluating cricothyroidotomy part-task simulation trainers
Dr Toby Winterbottom
Abstract TBC







